In recent times, the increased demand for healthcare services coupled with the spiralling costs of healthcare has brought the entire healthcare sector under the microscope. Stakeholders of the healthcare sector include:
(i) patients, who are both recipients of the healthcare service, as well as partial funders of the service through insurance premiums and direct payments to the service providers,
(ii) service providers such as doctors, hospitals, ancillary providers, pathology and radiology service providers, and
(iii) funders such as federal and state government health departments and private health insurers.
What is common to all these stakeholders is the need to contain costs and avoid wasteful expenditure, while ensuring high quality healthcare. In this context, data analytics can play a significant role in enabling cost-effective high quality service. Readers may be familiar with the oft quoted examples of how buying patterns of consumers help supermarkets to place popular items at the checkout counters, or how google uses our search terms to place related advertisements. In comparison, benefits of data analytics for the health sector can have a much larger impact as each and every one of us believe that quality healthcare is our birth right!
Creating effective analytics that produce actionable intelligence is particularly difficult in the healthcare sector, given the enormous complexity and variety of data and the many human factors that need to be considered.
Consolidating Healthcare Data
In Australia, public healthcare data is highly fragmented. However, private healthcare insurers (PHIs) hold data pertaining to at least the hospital-based healthcare services received by all their members. Examples of PHI data sources that can be used to compute cost and quality of care provided to (hospital) patients include:
(a) claims and billing data of providers, where providers include doctors, hospitals, and ancillary (e.g. dental, optical) service provider. Claims data hold details of the provider, the patient, the date of service, type of service provided (specified as Medical Benefits Schedule billing code), and charges for services provided;
(b) hospital admission and discharge data showing details of the admission and episode of care that includes patient demographics, ICD-10 diagnosis and procedure codes, length of stay, type of accommodation (example, ICU), prosthesis used etc.
In addition to the above, there are several data repositories that hold electronic health data, but these are outside the scope of this article.
Establishing a Baseline for Quality Healthcare
Once the data sources are identified, we need a set of robust analytical techniques to detect outliers that can effectively identify and measure variations in cost effective high quality healthcare services. The analytical techniques need to be complemented with appropriate visualisation techniques that can facilitate meaningful interaction with the data, offer explanations of the deviations and finally enable interpretation of the results within the healthcare service context. This calls for clear unambiguous definitions of a set of metrics that can reliably measure cost effective care.
Once a set of metrics are accepted by the different stakeholders of the healthcare community, we can intuit that all services that do not meet these well-defined metrics become genuine anomalies in service delivery. The way of assuring meaningful assessment of quality of service is by determining such anomalies in a consistent way and enabling reliable interpretation of comparative performance, which in turn can be actioned upon to improve effective quality of care.
A variety of data analytics techniques can be used to measure and compare health system performance. For example, statistical techniques, can analyse trends on high cost procedures such as hip and knee replacement procedures. Thus, develop objective measurable metrics to compare relative performance of medical providers as well as hospitals. Here performance is measured in terms of costs as well as quality of care factors such as readmission rate, infection rate, length of stay and so on. Techniques such as predictive modelling can predict expected hospital costs as well as length of stay for different types of procedures and these can be risk adjusted based on patient demographics and health status. Predictive models can go even further and give us indicators of what types of surgical procedures lead to higher infection and complication rates.
Continuing research moves on to explore complex relationships across providers and patients using the new area of social network analysis.
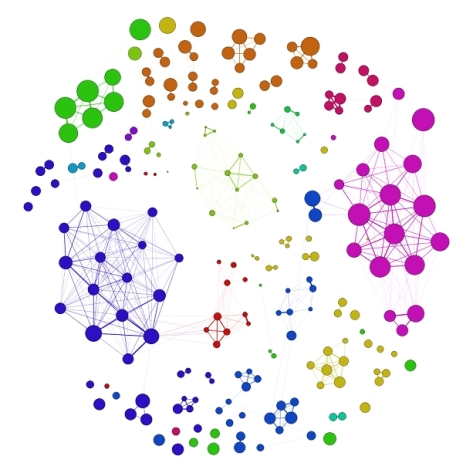
Figure 1 shows the pattern of sharing patients by a community of physiotherapy providers forming a “social network” of sorts. Each cluster of nodes indicates a close-knit community of providers who share common patients. The size of the nodes indicates the number of patients serviced by that provider and a thicker edge indicates a higher number of patients shared between providers in one week. The idea here is to explore any unusual behaviour patterns exhibited by a group of providers. An example of unusual behaviour would be, not just sharing a large number of patients, but sharing the same set of patients all the time, indicating either over-servicing, or a form of collusion among a group of providers and patients. Other network models could help in identifying effective team structures that could have a positive effect on patient’s outcome such as lower infection rates and lower recurring patterns of the problem.
Summary
To summarise, as far as the health sector is concerned, all analytics needs to be guided by a deep knowledge of the domain that involves understanding the problems of the stake holders, the work flow and information in the business, the codes used and their semantic representation within the context of the domain, for comparative measures of performance, where the cost may be monetary and the benefit could be another denomination like quality of care parameters such as reduced infection rate, reduce readmission rate, leading to better patient outcomes and cost effective care.
Further Reading
Details of some of the research work mentioned in this article can be seen at: http://www.cmc-is.com/
About the Author
Uma Srinivasan, PhD,
Lead Scientist at Capital Markets Cooperative Research Centre, Sydney, Australia, Health Market Quality Program

to the extent the wellbeing segment is concerned, all investigation should be guided by a profound learning of the area that includes understanding the issues of the dcotors, the work process and data in the business
LikeLike